Footnotes to 10 technologies
The 10 technologies are a TB vaccine, strep A vaccine, malaria mAb, bug to stop malaria, hep C vaccine, stroke drug, hep B cure, multipurpose diagnostic test, platform for programmable pandemic drugs, and a syphilis vaccine.
The fine print:
- 5 years from now means February 2nd, 2029.
- “Available” means “100,000 people have taken it”, except in the case of programmable drugs which I'll leave undefined (they're for possible future pandemics that haven't happened yet). You might argue that “approved by a regulator somewhere” is a more intuitive definition. That doesn’t count as available to me, because approvals don’t matter unless people actually use and benefit from a technology. There are often multi-year delays in getting new products to people who need them, and that’s part of what I want to complain about. In the other direction: perhaps a TB vaccine will only be impactful once tens or hundreds of millions of people have taken it; if it saves a life every 5,000 vaccine courses, 100,000 vaccinations sets the bar too low. That is largely true from a health impact point of view, but unfairly difficult to meet for a backwards-looking measure of success. By the time there are 100,000 administrations of a TB vaccine, we’ll be off to the races. (There will be 10,000+ administrations before 2029 in the M72 phase 3 clinical trial alone; that doesn’t yet count as off to the races, since we won’t know how well it works until the data from the trial is unblinded.)
- Arguably my title is misleading given my definition in footnote 2. "Exist” is different to "available". That said, grams of monoclonal antibodies against malaria have already been manufactured for use in clinical trials, so in some sense that product “exists”, we just don’t know how well it works yet or at what cost kilograms of it could be manufactured. In the important sense it doesn’t exist for people who might want it in Senegal, i.e. the sense of “availability” I defined above. I went back and forth on it, but decided that for most readers the title is likely to connote what I’m intending, so I kept it. You footnote people are sticklers though, so there’s my defence.
- TB vaccines are a “probably not” rather than a “no” because the VPM1002/Immuvac phase 3 in household contacts of TB patients being run in India may have a positive readout before 2029, perhaps even in 2024. The big M72/AS01E trial has not started enrolling; first results could come in early 2028. I’d be surprised if full results come before January 2029, and the current estimated completion date is August 2029, but it’s endpoint-driven so who knows! A regulatory submission on initial data is conceivable if the data is strong enough. I still can’t see a world where 100,000 people have received M72 by February 2nd 2029, even in my optimistic moods, but I hope I’m wrong.
- Strep A infections give kids strep throat all the time, and sometimes infections turn more dangerous than that, so a vaccine may well be a blockbuster product financially ($1bn/y+) if public health bodies decide to integrate one into regular schedules. But the large mortality number comes from complications following repeated infections, and in particular from rheumatic heart disease, more common in lower and middle income countries. There are few vaccines in the clinical pipeline, but the reason for that is in my view historical not scientific. The FDA banned development of a vaccine in the 1970s, lifted only in 2005/6, and that’s held back the field in terms of talent (scientific careers take decades to build) and conviction. In recent years there’s been a building wave again. There are lots of materials to learn more about the state of play on the SAVAC website; I'd start there.
- A reaction you may be having to half of this list is: how come we need vaccines for diseases that already have cures? On the flip, how come we need a cure for hep B when there’s already a great vaccine? Isn’t the problem lack of investment in public health and health systems, especially in lower and middle income countries, rather than the need for more technology? I have this reaction too, and for whatever reason it makes me particularly depressed when I think about malaria. Malaria is curable! If you make it to a clinic, it’s three days of drugs and you’ll probably be fine. Yet hundreds of thousands of kids still die of it every year, and hundreds of millions of people get infected. What the &@$#?! Really I should address this "why technology?" question in a standalone post some time, not a footnote, but my short answer is: public health investments vs tool development do not always require resource tradeoffs since the funding and talent pools for them differ, and if you're going after tools that make sense the two are usually synergistic. Circumstances differ across the world for the same disease, and more tools give health systems more options to work with. Nigeria would not be able to eradicate malaria with only the toolkit the U.S. had in the 1940s. The U.S. tried to eliminate syphilis starting in 1999, aiming for <1000 annual cases nationally, and has since given up. This week The New York Times told me there were 200,000 diagnosed cases of syphilis in the U.S. in 2022, up 80% since 2018. When I took the train to work last week I saw the ad below – in San Francisco, one of the richest counties in the world with an annual municipal budget exceeding $10,000 per person. Money and effort aren't always enough, when your toolset is limited. Public health bodies in San Francisco would love to have a syphilis vaccine in the arsenal alongside penicillin.

Church, syphilis, and Cliff's Variety (San Francisco, 2024) - Almost all kids under 5 in West Africa get drugs to prevent malaria in the rainy season, but the drugs are gross, not always swallowed, and they’re not always effective either. Imagine if you could get instant protection with one shot of the most potent antibodies instead? COVID can provide some inspiration. Not just for kids – monoclonals could be more useful than vaccines in a regional malaria outbreak where you want immediate protection (Florida…) instead of waiting for that ol' sluggish immune system to peak, or maybe safer for pregnant women than other options, or maybe useful for infants not yet eligible for vaccination that usually starts at 5 months, or maybe useful as protection after you get discharged from a treatment clinic from your last malaria case…
- The “(including rural)” here is meant to capture that bugs that stop malaria spreading already are available, they’re just not cost-effective at scale in rural areas of sub-Saharan Africa where continued releases of edited mosquitoes aren’t realistic. Things that would count in this row: gene drive, and this fungus discovered in mosquitoes around Lake Victoria. I.e. the “bugs” could be gene edited mosquitoes that get released, or could be microorganisms that get taken up by mosquitoes and affect malaria transmission. That second approach is in the process of working wonders for Wolbachia and dengue, another mosquito-borne disease.
- There are already cures for hepatitis C, and ambitious screen-and-treat programs using those are more important than developing a vaccine. Egypt showed you can virtually eliminate hep C that way. That said, more tools give you more options, and the populations affected in other countries tend to be different to Egypt (people who inject drugs, rather than older people infected by accident from contaminated needles in previous public health campaigns). Risk of reinfection is still meaningful in most places even if you’re cured, i.e. a vaccine would help.
- Incidentally, I went conservative on the hep C and hep B numbers. The two main sources that track the global burden of different diseases – IHME and the WHO – disagree significantly on hep C (540K vs 290K) and hep B (560K vs 820K). I took the lower number of each and rounded to 1 significant figure.
- Diet, exercise, and smoking affect your stroke risk, and stroke rates have happily gone down 75% over 60 years in the US mostly due to preventive measures. Statins probably help too, and I should drink less. Yet stroke is still the 5th biggest killer in the US, and treatment options once you have a stroke leave much to be desired. Clot-busters exist for ischemic stroke, to try and chemically disrupt the clot in your brain, but aren't used for most stroke events (see below) and would be actively harmful for hemorrhagic stroke patients. Mechanical intervention by ingenious-sounding surgery that starts at an artery by your groin and threads all the way up to grab the clot in your brain(!) works even better, but is limited by the number of skilled surgeons around. I asked my friend who's a doctor in a London hospital about it, and she recommended I time my stroke to 9am-5pm Monday to Friday when they offer the surgery. That's London! What hope do the rest of us have? We need simpler, safe drugs – and probably simpler/cheaper/portable CT scanners for use in more contexts around the world where clot-busters aren't on offer yet. Drugs that paramedics can give you to protect your brain while you travel to the hospital sound like the holy grail in theory, since there's less risk of harm than the clot-busters so you can give them in the "golden hour"... and in practice have failed 912 times. There’s got to be a way, there’s got to be a way…
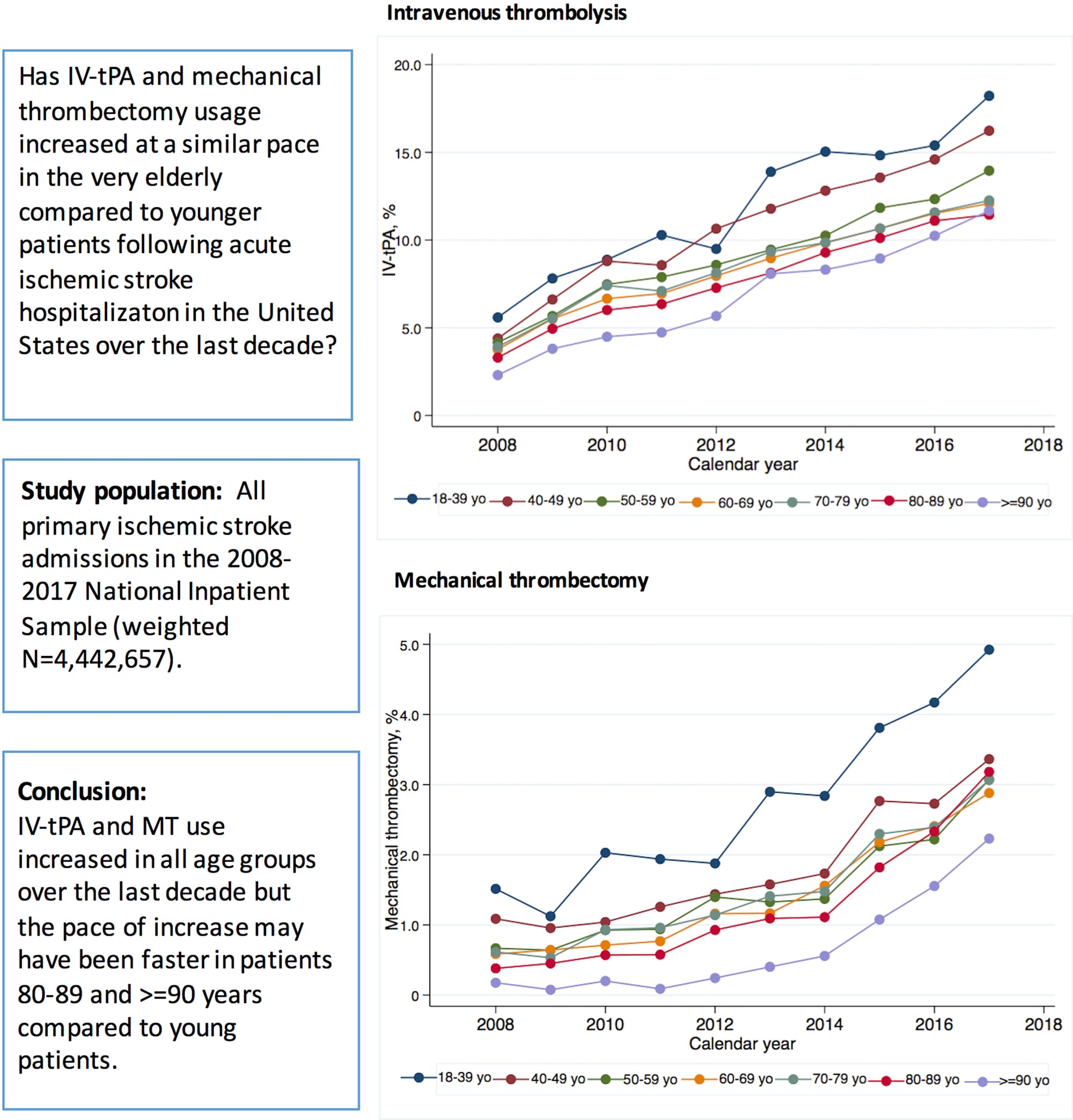
Clot-busters help but can only be used for some patients/strokes; surgery is even better but isn't widespread even in the U.S. (Source) - This isn’t a real footnote, just a comment that if you’ve made it this far down I bet it would be fun to talk some time. My professional and personal email addresses are what you’re most likely to guess for each. Send me a note saying hi.
- Hep B is controllable with drugs already, and seems wildly under-diagnosed and under-treated globally. Then there are many “functional cures” in the clinical pipeline (Table 1), some of which will hopefully prove even more useful. That’s wonderful. I’m holding a higher bar here: let’s get rid of the damn thing. Viral DNA hangs out in the nuclei of your liver cells even after existing treatments have gotten rid of most of what it spews off. It’s extremely hard to eradicate that pesky DNA without destroying too many of your own liver cells. But… it would be so cool. Could you create drugs that target only infected cells for destruction, at a pace your liver can take? Will improved CRISPR tools and even de novo DNA binding proteins help screw up the productive minichromosomes of viral DNA…? Probably not. Worth a shot.
- I would count success in the diagnostic row as: a multiplex diagnostic for at least 3 pathogens (i.e. flu + COVID does not count), available over the counter for use at home. Either a respiratory panel (e.g. flu + COVID + strep throat) or a fever panel (e.g. malaria + dengue + typhoid) would count. An at-home multiplex STI panel would be great (e.g. chlamydia + gonorrhea + syphilis), so I’d count that as a win too even though it doesn’t as intuitively meet the “tell you why you’re sick” phrasing. This one wouldn’t be as impactful as some of the other nine rows in the table, but it’s the product I’m most stunned doesn’t exist already. Even after a pandemic! The closest I'm aware of in the US is the Lucira COVID+flu test. It doesn't meet my definition since it's not multiplex enough, but it sounds great so I tried to get one from Amazon last time I was sick. Too late, as per the photo up top.
- By programmable drugs I’m referring to the colloquial sense of “drugs” (something you take when you’re sick to get better) not the medically precise term that would also include prophylactic vaccines. mRNA vaccines already count as programmable enough to me, so I give vaccines a checkmark. (Though accessibility of mRNA vaccines in many countries remains a significant unsolved problem.) I’m talking about getting something similar for therapeutics. A question remains of how many future pandemic threats the platform would have to cover for it to “count”, since no platform can cover everything. I would count this row as achieved if something like locked nucleic acids (LNAs) worked out, even if they’re “only” useful against single strand RNA viruses. That would cover flus and coronaviruses and I’d be a happy camper.
- Source for 7M-25M excess COVID deaths.
- Syphilis is easily curable with penicillin, but it doesn't always make you feel sick. If you don't know you're infected, and you get pregnant, it is likely to lead to a miscarriage, stillbirth, or infant death. Syphilis prevalence is poorly measured globally, but in some countries seems to be as high as 3%. The top priority today should be to provide tests and treatment for women in their first antenatal care visit; for many countries that means switching from rapid HIV tests to the cheap (<$1) dual HIV/syphilis rapid tests. However, modeling suggests that won't be enough on its own, in part because women can get reinfected by the same partner after they're cured. A vaccine would help prevent that, and might slash congenital syphilis rates.
- The R21/Matrix-M collaboration between Oxford University, research centres in Burkina Faso, Mali, Tanzania, and Kenya, and the Serum Institute of India, has been an interesting example to watch of a university working with a close commercial partner, without much in the way of product development intermediaries or philanthropy (though Open Phil supported the 5 trial sites for the phase 3 with $2.5M around the edges). The speed of clinical development for R21 has been unusual in the sector, and makes me wonder what other partnerships like that could work.
- $10 billion over 10 years might be a little light given how expensive clinical trials are, but it would genuinely move the needle on some of these problems. The two numbers I think about most often in relation to these high level resource allocation questions are: $4 billion per year, and $16.8 billion needed by 2035. $4 billion per year refers to how much the canonical tracker of neglected disease R&D, G-FINDER, estimates is spent globally on that R&D. The $16.8 billion number refers to what this paper estimates it would cost to get 147 products in the neglected disease pipeline approved by 2035, averting 26.9M future deaths. Not all the diseases I listed in this post would qualify as neglected in this sense, since they affect people in high income countries too. But adding $1 billion per year to the $4 billion is ambitious yet absorbable; and spending $10 billion of that crude $16.8 billion estimate would indeed lead to millions of lives being saved.
Thanks to Sangeeta Bhatia and Mireille Kamariza for comments